FARAPULSE PFA is proven, safe, and effective in studies across the globe.
FARAPULSE PFA treats atrial fibrillation (AFib) without causing injury to nearby non-cardiac tissue. Backed by the most extensive clinical research in Pulsed Field Ablation, it delivers safety and performance you can have confidence in.
Proven2
patients treated worldwide
clinical trials and 150+ publications
Safe1
real-world major adverse event rate (N=17,642)*
reports of esophageal fistula or dysmotility, pulmonary vein stenosis, or persistent phrenic nerve injury
Effective
showed no recurrence of AFib symptoms at 1 year3†
remained free of antiarrhythmic medications at 1 year4
FARAPULSE PFA is approved for both paroxysmal and persistent AFib patients.
FARAPULSE PFA delivered outstanding outcomes across patient types. AFib recurrence and symptoms were minimized, and atrial arrhythmia burden was reduced.3-5
Cardiac ablation: proven to slow AFib progression.6,7
As AFib progresses, recurrent episodes increase the risk of stroke, clots, and heart failure.8 Cardiac ablation is the only therapy shown to significantly reduce AFib progression.6,7
Clinical advantages of cardiac ablation for AFib
In studies comparing ablation with antiarrhythmic drugs (AADs), ablation is associated with:9-14
Fewer AFib recurrences
Lower mortality rates
Fewer heart failure–related hospitalizations
Reduced need for cardioversion
Reduction in AFib symptoms (palpitations, fatigue, and effort intolerance)
FARAPULSE PFA is transforming AFib treatment.
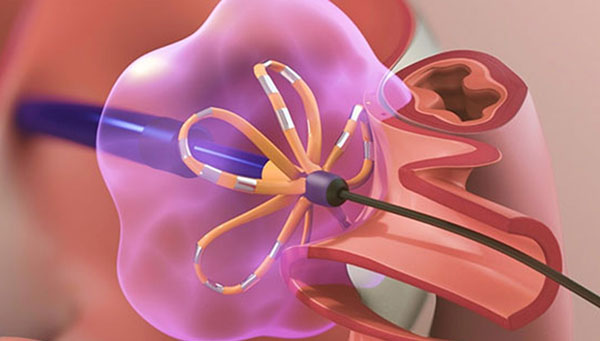
FARAPULSE Pulsed Field Ablation (PFA) differs from thermal ablation. Serious adverse events seen in thermal ablation like esophageal fistual, pulmonary vein stenosis, or persistent phrenic nerve injury were not reported with FARAPULSE PFA.1
Traditional Cardiac Ablation
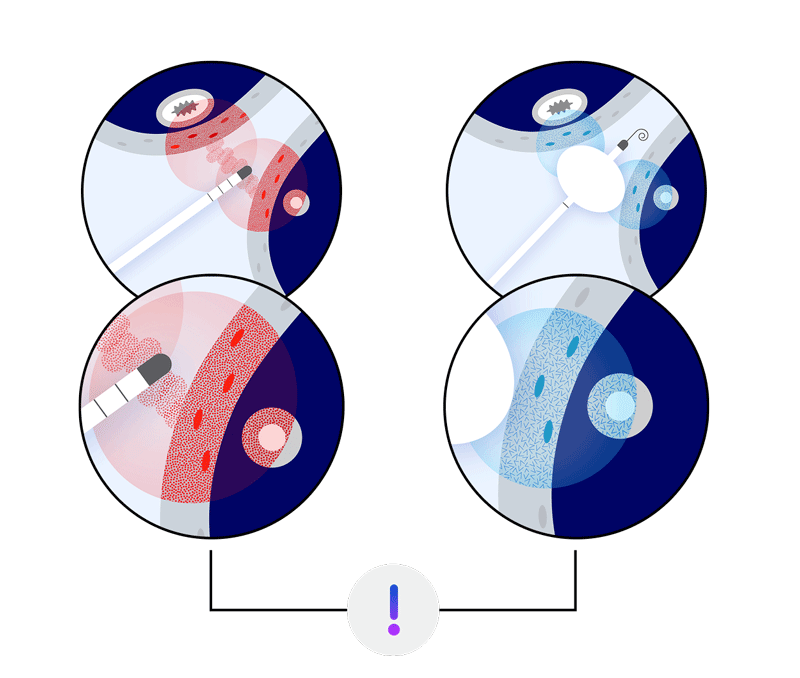
Hot or cold thermal energy can cause collateral damage to esophagus or phrenic nerve.
FARAPULSE PFA
Non-thermal, cardiomyocyte-selective electrical energy avoids damage to adjacent areas.
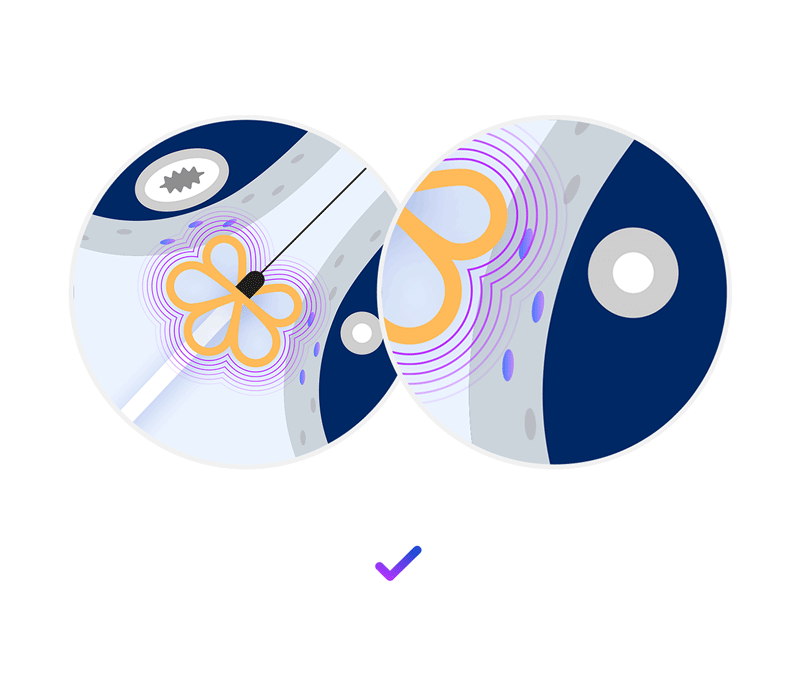
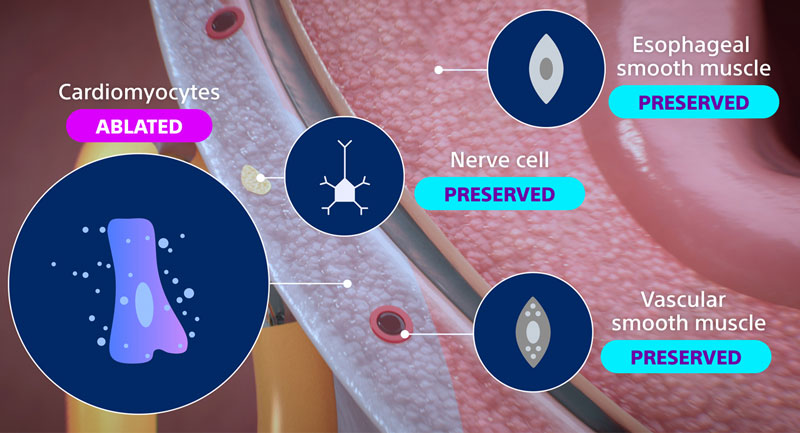
PFA in action: selective electroporation of cardiac tissue.
PFA preferentially electroporates cardiomyocytes. Other cell types—like nerve and esophageal tissue—are resistant to its effects, reducing the risk of collateral injury.
Patients reported positive outcomes in satisfaction, activity, and peace of mind.
At 1 year post-procedure, patients reported enhanced quality of life.2,4
were hardly bothered by AFib symptoms (palpitations, irregular beats, light-headedness)
reported improved ability to participate in sports, hobbies, and recreation
were very satisfied with AFib control and symptom relief
reported AFib no longer limited their lives
Helpful resources
Get a detailed clinical overview of FARAPULSE.
Connect with us for additional information.
Locate centers performing the FARAPULSE procedure.
References:
1. Ekanem E, Neuzil P, Reichlin T, et al. Safety of pulsed field ablation in more than 17,000 patients with atrial fibrillation in the MANIFEST-17K study. Nat Med. 2024;30:2020–2029. https://doi.org/10.1038/s41591-024-03114-3
2. Boston Scientific. Data on file.
3. Turagam MK, Neuzil P, Schmidt B, et al. Safety and effectiveness of pulsed field ablation to treat atrial fibrillation: one-year outcomes from the MANIFEST-PF registry. Circulation. 2023;148(1):35–46.
4. Reddy VY, Gerstenfeld EP, Natale A, et al. Pulsed field or conventional thermal ablation for paroxysmal atrial fibrillation. N Engl J Med. 2023;389(18):1660–1671. doi:10.1056/NEJMoa2307291
5. Reddy VY, Gerstenfeld EP, Schmidt B, et al. Pulsed Field Ablation of Persistent Atrial Fibrillation With Continuous ECG Monitoring Follow-Up: ADVANTAGE AF-Phase 2. Circulation. Published online April 24, 2025. doi:10.1161/CIRCULATIONAHA.125.074485
6. Kuck KH, Lebedev DS, Mikhaylov EN, et al. Catheter ablation or medical therapy to delay progression of atrial fibrillation: the randomized controlled atrial fibrillation progression trial (ATTEST). Europace. 2021;23(3):362–369. doi:10.1093/europace/euaa298
7. Benali K, et al. Catheter ablation of paroxysmal atrial fibrillation and disease progression: magnitude of the antiprogression effect and role of intervention timing. Heart Rhythm. 2025;0(0).
8. Shah AJ, Hocini M, Komatsu Y, et al. The Progressive Nature of Atrial Fibrillation: A Rationale for Early Restoration and Maintenance of Sinus Rhythm. J Atr Fibrillation. 2013;6(2):849. Published 2013 Aug 31. doi:10.4022/jafib.849
9. AlTurki A, Proietti R, Dawasaz AA, Altawil M, Di Biase L, Natale A. Catheter ablation for atrial fibrillation in heart failure with reduced ejection fraction: a systematic review and meta-analysis of randomized controlled trials. BMC Cardiovasc Disord. 2019;19(1):18.doi:10.1186/s12872-019-0990-2
10. Asad ZUA, Yousif A, Khan MS, et al. Catheter ablation versus medical therapy for atrial fibrillation: a systematic review and meta-analysis of randomized controlled trials. Circ Arrhythm Electrophysiol. 2019;12(9):e007414. doi:10.1161/CIRCEP.119.007414
11. Khan SU, Rahman H, Talluri S, Kaluski E. Catheter ablation and mortality and morbidity in atrial fibrillation: a systematic review and meta-analysis. JACC Clin Electrophysiol. 2018;4(5):626–635. doi:10.1016/j.jacep.2018.01.012
12. Chen C, Zhang Y, Liang Z, et al. Effect of catheter ablation versus antiarrhythmic drugs on cognitive function in atrial fibrillation patients. J Interv Card Electrophysiol. 2018;52(1):9–18.
doi:10.1007/s10840-018-0346-6
13. Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275–e444. doi:10.1016/j.
14. Allan KS, Aves T, Henry S, Banfield L, Victor JC, Dorian P, Healey JS, McGillion MH. Health-related quality of life in patients with atrial fibrillation treated with catheter ablation or antiarrhythmic drug therapy: a systematic review and meta-analysis. CJC Open. 2020;2(4):286–295. doi:10.1016/j.cjco.2020.02.008
*In a clinical trial the major adverse event rate was 0.98% (N=17,642). Due to the retrospective nature of the registry, the adverse event rate was not reported at a prespecified time point. Serious adverse events include atrioesophageal fistula, pulmonary vein stenosis, or persistent phrenic nerve injury.
†In a clinical trial 81.6% of people with paroxysmal AFib had no atrial fibrillation, atrial flutter, or atrial tachycardia after a single ablation procedure at 12 months.