First PFA Study in Persistent AFib Patients (N=255)1
At 29 US sites, 49 operators conducted 1-year continuous ECG monitoring with insertable cardiac monitors (ICMs) to provide detailed analysis of atrial arrhythmia burden reduction.
STUDY DESIGN
Multicenter, prospective, single-arm, IDE study
PATIENT POPULATION
Drug–refractory persistent AFib
REPORTED OUTCOMES
Safety, efficacy, atrial arrhythmia (AA) burden
FARAPULSE PFA proved to be effective in a hard-to-treat population.
Outcomes at 3 Months and 1 Year Post-Ablation
SAFETY
2.4%
safety event rate
at 3 months*
0
reported cases of pulmonary vein stenosis, atrioesophageal fistula, or phrenic nerve palsy
PRIMARY EFFICACY
73.4%
event-free rate at 12 months†
81%
remained free from symptomatic recurrence at 12 months
RECURRENCE
52%
had no recurrence over 12 months
Of those who had recurrence:
had no episodes >1 hour
had no episodes >24 hours
Low atrial arrhythmia (AA) burden resulted in low healthcare utilization (HCU) in advanced AFib patients.
The impact of AA burden: a clinically meaningful endpoint.
The traditional definition for recurrence in trials—episodes ≥30 seconds—may not reflect clinically meaningful AFib.2 AA burden, by contrast, is a sensitive, patient-centric measure of AFib control and treatment success across healthcare utilization (HCU) and quality of life.1
AA Burden and Healthcare Utilization (HCU) at 1 Year
AA BURDEN
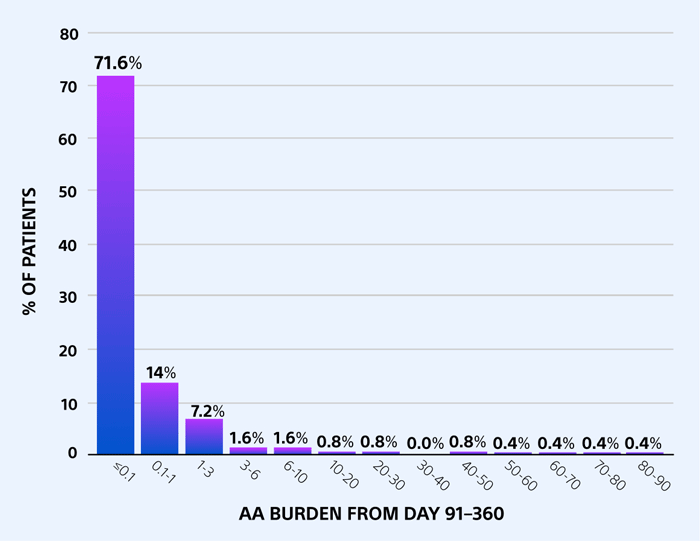
71.6% of patients had ≤0.1% AA burden
HCU by AA BURDEN
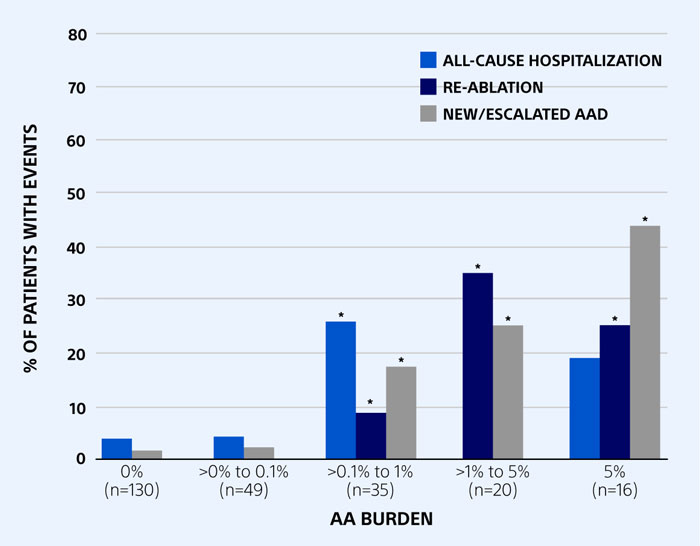
*p<0.0125 compared to 0% burden group
AA burden <0.1% linked to lower HCU vs. AA burden >0.1% (p<0.0125)
LONGEST AA EPISODE
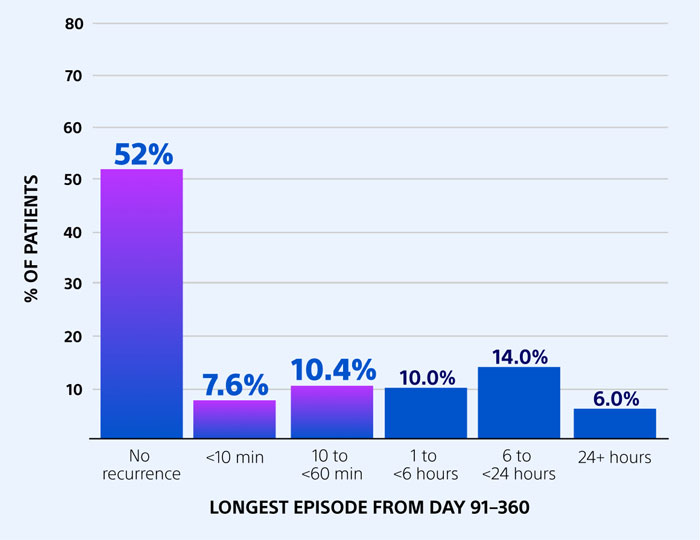
52% of patients had no AA recurrence 70% experienced AA episodes <1 hour
HCU by LONGEST AA EPISODE
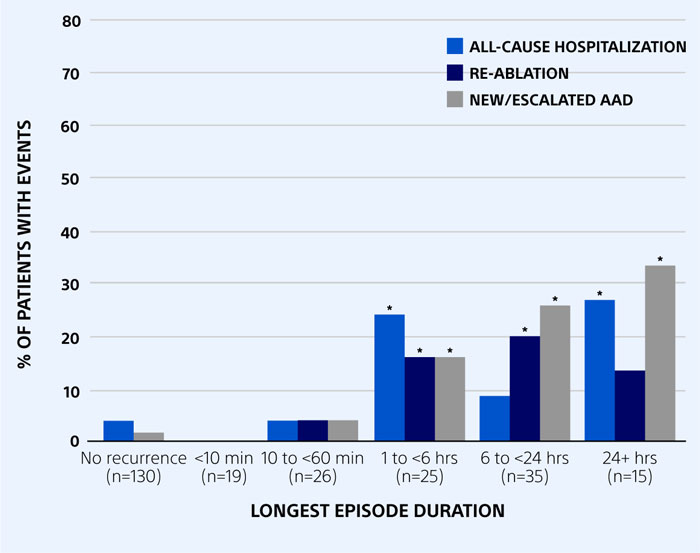
*p<0.01 compared to no recurrence group
No AA recurrence linked to lower HCU vs. episodes >1 hour (p<0.01)
HCU was over tenfold higher in patients with AA burden >0.1% or episodes lasting >1 hour
Key Takeaways
- FARAPULSE PFA met primary safety and efficacy endpoints with a low rate of major events
- The majority of patients had virtually no AA burden at 12 months, associated with lower HCU
- The majority of patients had no AA recurrence; of those that did, 70% had episodes <1 hour
Next: See how FARAPULSE compares with cryoablation.
References:
1. Reddy VY, Gerstenfeld EP, Schmidt B, et al. Pulsed field ablation of persistent atrial fibrillation with continuous ECG monitoring follow-Up: ADVANTAGE AF-Phase 2. Circulation. Published online April 24, 2025. doi:10.1161/CIRCULATIONAHA.125.074485
2. Steinberg JS, O’Connell H, Li S, Ziegler PD. Thirty-second gold standard definition of atrial fibrillation and its relationship with subsequent arrhythmia patterns: analysis of a large prospective device database. Circ Arrhythm Electrophysiol. 2018;11(7):e006276. doi:10.1161/CIRCEP.118.006276
*Adverse events included cardiac tamponade or perforation (n=1), pulmonary edema (n=1), death (n=1), PFA system- or procedure-related cardiovascular or pulmonary event (n=2), stroke (n=3), and vascular access complication (n=1).
†Most common chronic treatment failure event was documented recurrence of a sustained atrial arrhythmia (atrial fibrillation, atrial flutter, atrial tachycardia).