FARAPULSE PFA vs. Standard Thermal Ablation in Paroxysmal AFib Patients (N=607)1
At 30 US centers, 65 operators conducted 1:1 randomization to FARAPULSE PFA or thermal ablation, using either radiofrequency ablation (RFA) or cryoballoon ablation (CBA) at each site.
STUDY DESIGN
Multicenter, prospective, single-blind, randomized controlled study
PATIENT POPULATION
Drug–refractory paroxysmal AFib
REPORTED OUTCOMES
Safety, efficacy, non-inferiority to thermal ablation
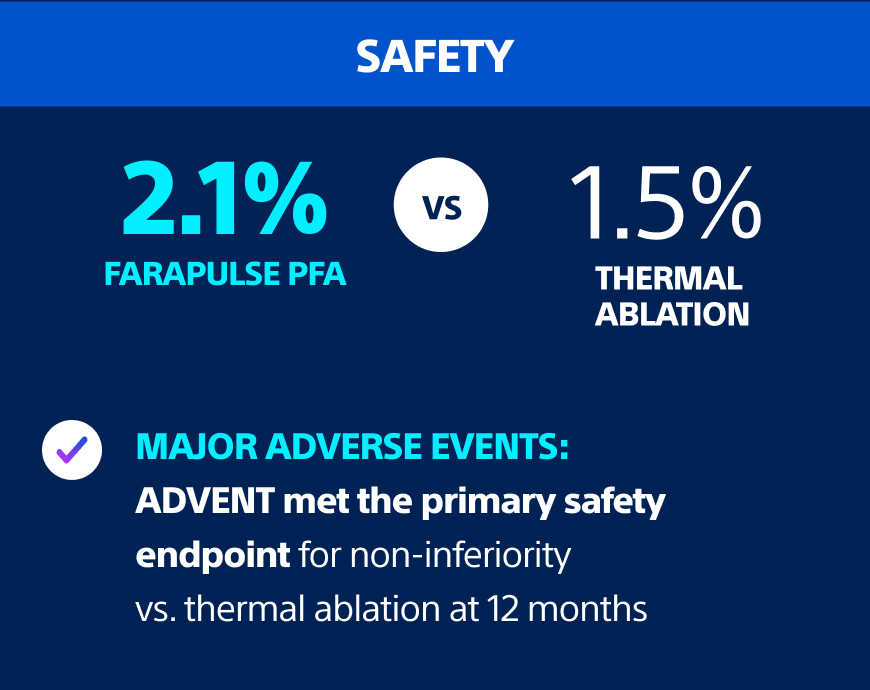
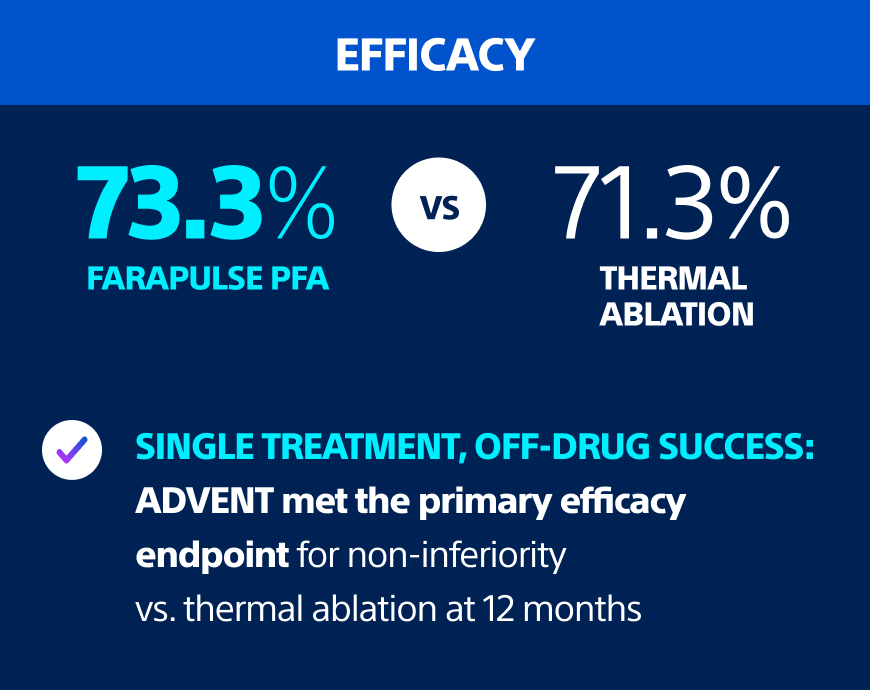
FARAPULSE PFA delivered excellent outcomes comparable to thermal ablation.
Outcomes at 1 Year Post-Ablation
Significantly more patients achieved minimal atrial arrhythmia (AA) burden with FARAPULSE PFA.
The impact of AA burden: a clinically meaningful endpoint.
The traditional definition for recurrence in trials—episodes ≥30 seconds—may not reflect clinically meaningful AFib.2 AA burden, by contrast, is a sensitive, patient-centric measure of AFib control and treatment success across healthcare utilization (HCU) and quality of life.1
AA Burden at 1 Year3
Post-Ablation AA Burden Threshold of 0.1% by Modality
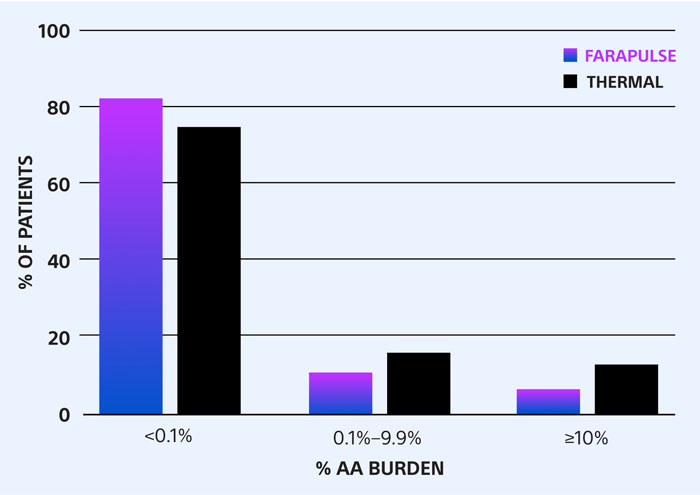
FARAPULSE PFA-treated patients were significantly more likely to have AA burden <0.1%
HCU is significantly lower with AA burden <0.1% vs. ≥10%3
Rate of Healthcare Utilization
| AA Burden | <0.1% | 0.1%–9.9% | ≥10% |
| Redo Ablations | 0.86% | 11.1% | 38.3% |
| Cardioversions | 0.65% | 9.9% | 17% |
| Hospitalizations | 1.72% | 14.8% | 42.6% |
Quality of life is significantly higher with AA burden <0.1% vs. ≥10%3
Fewer symptoms
More participation in activities
Fewer treatment concerns
Greater treatment satisfaction
Key Takeaways
- FARAPULSE PFA met all primary and secondary endpoints for safety and efficacy
- FARAPULSE PFA patients were significantly more likely to have AA burden <0.1% vs. those treated with thermal ablation
- AA burden <0.1% translated to signifcantly greater quality of life and lower risk for redo ablation, cardioversion, and hospitalization
References:
1. Reddy VY, Gerstenfeld EP, Natale A, et al. Pulsed field or conventional thermal ablation for paroxysmal atrial fibrillation. N Engl J Med. 2023;389(18):1660–1671. doi:10.1056/NEJMoa2307291
2. Steinberg JS, O’Connell H, Li S, Ziegler PD. Thirty-second gold standard definition of atrial fibrillation and its relationship with subsequent arrhythmia patterns: analysis of a large prospective device database. Circ Arrhythm Electrophysiol. 2018;11(7):e006276. doi:10.1161/CIRCEP.118.006276
3. Reddy V, Mansour M, Calkins H. et al., Pulsed Field vs Conventional Thermal Ablation for Paroxysmal Atrial Fibrillation: Recurrent Atrial Arrhythmia Burden. J Am Coll Cardiol. null2024, 0 (0). https://doi.org/10.1016/j.jacc.2024.05.001